Medicaid basics
History
On July 30, 1965, President Lyndon B. Johnson signed into law legislation that led to the establishment of Medicare and Medicaid. Together, these programs currently provide health care coverage to about 42 percent of the nation’s population, with Medicaid serving 24 percent.1
Today, Medicaid is the nation’s single largest health care insurer, covering approximately 79.4 million people in the United States in 2017 — more than one million of whom live in Minnesota.2
Currently, the federal government shares financial responsibility for the Medicaid program by matching state costs with federal dollars. While certain federal requirements outline who and what must be covered in each program, states generally have flexibility to tailor and expand their Medicaid program to meet the needs of their population and state budgets.
In 1966, Minnesota implemented the state’s Medicaid program, which is called Medical Assistance. Today, it covers one out of every five Minnesotans. As the third largest insurer in the state after self-insured employer-based coverage and Medicare, it makes up nearly 16 percent of the state’s health insurance market.
Who is eligible?
Minnesotans may enroll in Medicaid in Minnesota if they meet certain eligibility requirements under the following categories:
- Parents and children
- Age 65 or older, blind or have disabilities
- Adults
Medicaid enrollees must demonstrate their program eligibility at least once a year. An individual’s eligibility is determined by factors such as household income, family size, age, disability status, and citizenship or immigration status. These criteria are set by federal and state law and vary by category.
To access more detailed information about income eligibility limits in Minnesota’s Medicaid program, see the income and asset guidelines.
How are Medicaid services purchased and delivered?
The most common methods of payment in Medicaid programs:
- Fee for service, where the state directly pays providers a flat fee for each service delivered.
- Managed care, where the state contracts with health plans and pays them a monthly per member capitation payment to provide all covered services.
Other payment arrangements with providers, care systems and partner organizations, referred to as accountable care organizations or models, are also growing in Medicaid as the health care system moves to pay for better health outcomes. A few states have implemented innovative models of service delivery and provider payment — such as Minnesota’s Integrated Health Partnerships — to reduce overall costs while improving enrollee outcomes.
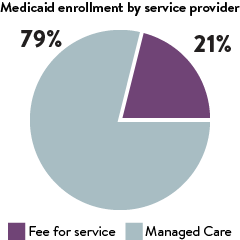 Most Minnesotans enrolled in Medicaid receive services through health plans or managed care organizations. The remaining enrollees receive services through the traditional fee-for-service system, where providers receive a payment from DHS directly for each service provided to an enrollee. Fee-for-service enrollees may choose from any provider enrolled in the Medicaid program.
Most Minnesotans enrolled in Medicaid receive services through health plans or managed care organizations. The remaining enrollees receive services through the traditional fee-for-service system, where providers receive a payment from DHS directly for each service provided to an enrollee. Fee-for-service enrollees may choose from any provider enrolled in the Medicaid program.
In 2018, about 234,000 people were enrolled in the state’s fee-for-service system in any given month with just over 883,000 people enrolled in health plans.
See the map of health plans serving Medicaid families in children by county.
- Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Expenditures: 2016, Table 22. Accessed on Jan. 17, 2017, at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html.
- ibid.

